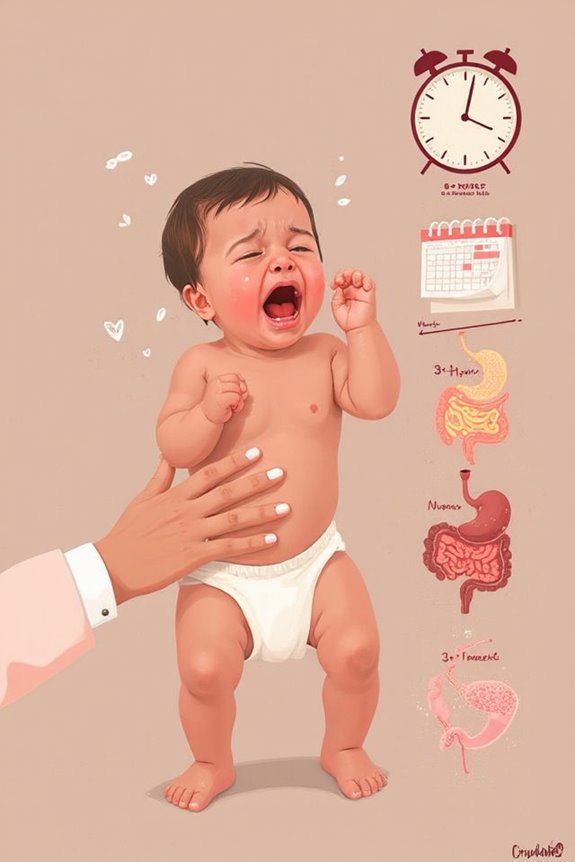
Colic affects 10-40% of babies, characterized by intense crying for 3+ hours daily, 3+ days weekly, lasting 3+ weeks. You’ll notice symptoms like evening crying peaks, flushed face, clenched fists, and arched back. Causes may include immature nervous systems, digestive discomfort, or food sensitivities. Soothing techniques include swaddling, white noise, and gentle motion. Dietary changes for breastfeeding mothers or specialized formulas can help. The following strategies offer relief during this challenging but temporary phase.
Key Takeaways
- Colic involves unexplained crying for more than three hours daily on three or more days per week for at least three weeks.
- Potential causes include digestive system development, gut bacteria imbalance, and possible food sensitivities or allergies.
- Most colicky babies show physical signs like flushed face, tight fists, arched back, and swollen belly during episodes.
- Effective soothing techniques include swaddling, white noise machines, gentle motion, and responsive rocking.
- Dietary adjustments like eliminating allergens for breastfeeding mothers or specialized formulas may reduce colic symptoms.
What Is Colic? Defining This Common Infant Condition
Frustration often fills a home when a baby cries inconsolably for hours on end. This phenomenon, known as colic, affects between 10-40% of infants regardless of gender or feeding method.
The medical colic definition includes three key criteria:
- Crying for more than three hours daily
- Episodes occurring more than three days weekly
- Condition persisting for more than three weeks
I’ve observed that colicky infant crying typically follows a pattern: beginning around two weeks of age, peaking at six weeks, and resolving by 12-16 weeks. Episodes most commonly occur in the evening.
It’s important to understand that colic rarely indicates any serious underlying condition—fewer than 5% of excessive crying cases stem from organic disease. While stressful in the moment, colic generally resolves without long-term complications.
Signs and Symptoms: How to Recognize Colic in Your Baby

Recognizing colic in your baby involves looking for specific patterns rather than just isolated crying spells. The classic colic symptoms follow the “rule of threes”: crying for more than 3 hours daily, occurring more than 3 days weekly, for at least 1 week.
Look for these key crying patterns:
- Episodes typically peak between 6 p.m. and midnight
- High-pitched, loud wailing that sounds urgent or distressed
- Physical signs including flushed face, clenched fists, and arched back
- Tight or swollen belly with legs pulled toward abdomen
- Resistance to typical soothing methods
Unlike regular fussiness, colicky babies are extremely difficult to console. These symptoms generally peak around six weeks of age and resolve by 3-4 months. If you’re concerned, tracking your baby’s crying episodes can help your doctor determine if it’s colic.
Potential Causes: Theories Behind Infantile Colic

While researchers haven’t pinpointed an exact cause of colic, several theories attempt to explain this challenging condition that affects so many families. Current research points to multiple possible factors:
Sensitivity Factors
- An immature nervous system that struggles with self-soothing
- Heightened sensitivity to environmental stimuli like lights and sounds
- Individual temperament differences affecting adaptation abilities
- Family stress potentially influencing infant behavior patterns
Gastrointestinal Theories
- Developing digestive system causing discomfort
- Imbalances in gut bacteria (microbiome)
- Possible food allergies or intolerances, particularly to cow’s milk protein
- Improper feeding techniques leading to gas or discomfort
These theories are supported by correlational evidence, though none has been definitively proven. The “fourth trimester theory” suggests colic may simply represent a difficult adjustment to life outside the womb.
The Rule of Three: Diagnosing Colic in Newborns
Three key markers form the foundation of colic diagnosis, creating what pediatricians commonly call the “Rule of Three.” When your baby cries intensely for more than three hours daily, continues this pattern for more than three days weekly, and maintains these symptoms for longer than three weeks, doctors can confidently diagnose colic.
These diagnostic criteria help distinguish colic from other conditions that might cause excessive crying. During a clinical assessment, your pediatrician will:
- Evaluate your baby’s crying patterns
- Perform a thorough physical examination
- Rule out other medical conditions
When applying these criteria, it’s essential to recognize that colicky babies are otherwise healthy and well-fed. The condition typically resolves by 3-6 months of age with no long-term health effects.
Soothing Strategies: Effective Techniques for Calming Colicky Babies

Parents dealing with a colicky baby need practical, reliable methods to provide relief during those challenging crying episodes. I recommend starting with responsive techniques like swaddling and gentle rocking, which offer temporary comfort to distressed infants.
White noise machines can greatly reduce crying durations and improve sleep patterns by mimicking sounds from the womb. Motion strategies, such as car rides or vibrating chairs, often calm babies due to their soothing movement and ambient noise.
Consider these additional approaches:
- Sensory stimulation through gentle massage
- Pacifier use to help satisfy the natural sucking reflex
- Creating a calm environment with dimmed lights
- Maintaining comfortable room temperature
Remember that while these methods won’t cure colic, they can make episodes more manageable for both you and your baby.
Dietary Considerations for Breastfeeding Mothers and Formula-Fed Babies
Because a baby’s digestive system is still developing, what mothers eat and the formula choices parents make can greatly impact colic symptoms. If you’re breastfeeding, consider these dietary adjustments:
- Eliminate common allergens like cow’s milk, eggs, and wheat from your diet
- Reduce FODMAPs (fermentable carbohydrates found in certain fruits and vegetables)
- Avoid cruciferous vegetables such as broccoli and cabbage
- Stay well-hydrated to maintain milk supply
For formula-fed infants, specialized formula options may help:
- Hypoallergenic formulas with partially broken-down proteins
- Elemental formulas for babies with severe allergies
- Fermented formulas that may be gentler on sensitive digestive systems
Research shows that while not all dietary changes work for every baby, targeted elimination of trigger foods can greatly reduce colic symptoms in many infants.
When to Seek Medical Help: Red Flags Beyond Normal Colic
While dietary changes often help reduce colic symptoms, recognizing when crying goes beyond normal colic is essential for your baby’s health and safety. I want to help you identify red flag symptoms that require immediate medical evaluation:
- Fever of 100.4°F (38°C) or higher
- Changes in breathing patterns or effort
- Increased irritability when held or touched
- Vomiting or diarrhea
- Unusual-sounding cry
These signs could indicate serious conditions like ear infections, meningitis, or bacteremia, rather than simple colic. Other concerning behaviors include:
- Excessive crying that cannot be soothed
- Unusual sleepiness or sluggishness
- Pale or bluish skin color
- Changes in feeding patterns
Trust your instincts—if you’re worried about your baby’s condition, contact your healthcare provider immediately.
Coping as Parents: Managing Stress During the Colic Phase
Living through your baby’s colic phase can feel like an endless marathon of crying, sleepless nights, and emotional exhaustion. Research shows that both mothers and fathers experience significant stress during this challenging time.
Effective stress management is essential for your wellbeing and your ability to care for your baby. Consider these approaches:
- Seek emotional support from family, friends, or parenting groups
- Practice self-care through exercise or hobbies
- Share childcare responsibilities with your partner
- Consider professional counseling if you feel overwhelmed
Remember that paternal stress often mirrors maternal stress, making support for both parents vital. The good news? Most colic resolves by three to four months, and the anxiety you’re feeling is typically short-lived with no long-term effects on your mental health.
Frequently Asked Questions
Can Colic Affect a Baby’s Long-Term Development?
I believe colic doesn’t typically have a significant long-term impact on your baby’s development. Most colicky babies achieve their developmental milestones normally once the condition resolves around 3-4 months of age.
Are Colicky Babies More Likely to Develop Other Health Conditions Later?
Facts find favorable news: colic itself doesn’t increase health risks long-term. Based on research, I can assure you that while colic implications are stressful now, they don’t predispose your baby to poorer health outcomes later in life.
Do Specific Ethnic Groups Experience Higher Rates of Colic?
I’ve found that ethnic groups don’t greatly differ in colic rates. While cultural practices might affect how it’s reported and managed, there’s no strong evidence suggesting any genetic predisposition across ethnic backgrounds.
Can Colic Skip a Generation or Run in Families?
While 30% of babies experience colic, I can tell you there’s no strong evidence for genetic predisposition or familial patterns. Colic doesn’t directly run in families or skip generations like some hereditary traits do.
Does Birth Order or Delivery Method Influence Colic Development?
I’ve found that birth order may influence colic, with some studies showing higher rates in babies with siblings. However, delivery method doesn’t seem to affect colic development based on current research.
References
https://www.ncbi.nlm.nih.gov/books/NBK518962/
https://www.aafp.org/pubs/afp/issues/2015/1001/p577.html
https://www.childrenshospital.org/conditions/colic
https://www.mayoclinic.org/diseases-conditions/colic/symptoms-causes/syc-20371074
https://jpedres.org/articles/infantile-colic-in-infants-aged-one-six-months-and-the-practices-of-mothers-for-colic/doi/jpr.galenos.2019.72687
https://my.clevelandclinic.org/health/diseases/10823-colic
https://www.nyp.org/pediatrics/digestive-diseases/motility-disorders/colic
https://en.wikipedia.org/wiki/Baby_colic
https://www.hopkinsmedicine.org/health/conditions-and-diseases/colic
https://www.nhs.uk/conditions/colic/





