Babies get ear infections primarily because of their unique anatomy. Their Eustachian tubes are shorter, more horizontal, and have less developed muscles than adults, making drainage difficult. Infections typically start when viruses or bacteria enter these tubes during colds or respiratory illnesses. Environmental factors like secondhand smoke and daycare exposure increase risks. Watch for signs like ear tugging, irritability, fever, or disturbed sleep. Understanding these fundamentals can help you spot potential problems before they worsen.
Key Takeaways
- Babies’ shorter, more horizontal Eustachian tubes allow easier entry of pathogens into the middle ear.
- Viral and bacterial infections from colds or respiratory illnesses commonly spread to the ear.
- Immature immune systems make babies less capable of fighting off infections that reach the ear.
- Exposure to cigarette smoke, daycare attendance, and allergies increase infection risk.
- Poor drainage from underdeveloped ear structures causes fluid buildup where infections thrive.
Anatomy of Baby Ears: Why They’re Prone to Infection
While adults experience ear infections occasionally, babies are particularly susceptible due to their unique ear anatomy. The primary culprit is the Eustachian Tube, which connects the Middle Ear to the back of the throat.
In infants, this tube has critical differences:
- Shorter length and more horizontal orientation
- Less developed muscles controlling tube opening
- Poorer drainage capabilities
These structural differences create a more direct pathway for bacteria and viruses to travel from the throat to the middle ear. Additionally:
- The infant’s Middle Ear cavity is smaller
- Their eardrums are thinner and more delicate
- Mastoid air cells (air spaces behind the ear) are less developed
Combined with an immature immune system, these anatomical factors explain why babies experience ear infections much more frequently than adults.
Common Causes of Ear Infections in Infants

Because a baby’s ear anatomy differs markedly from an adult’s, they’re much more vulnerable to developing ear infections from various sources. The primary culprits behind these painful episodes include:
- Viral infections – Most ear infections stem from common viruses that spread easily among children
- Bacterial infections – Organisms like Streptococcus pneumoniaeand *Haemophilus influenzae* frequently cause ear infections
These pathogens often enter a baby’s system during colds or respiratory infections, when the eustachian tubes become blocked with mucus. Environmental factors also play a significant role:
- Exposure to cigarette smoke
- Daycare attendance (increased germ exposure)
- Allergic reactions that cause inflammation
Breastfeeding can provide protective antibodies against these infections, while timely vaccinations help prevent specific bacterial causes.
Warning Signs: Recognizing Ear Infection Symptoms

Spotting an ear infection in your baby requires careful attention to subtle cues they can’t verbalize. Symptom recognition is critical, as ear infections develop rapidly, especially in babies 6-24 months old.
Watch for these behavioral indicators:
- Ear tugging or pulling
- Difficulty sleeping or lying down
- Fever (100°F or higher)
- Crying more than usual
- Reduced appetite or trouble feeding
Physical symptoms include:
- Fluid drainage from the ear
- Balance problems
- Reduced response to sounds
Seek immediate medical attention if you notice:
- High fever or severe pain
- Bloody or pus-like discharge
- Symptoms lasting more than a day
- Any ear infection signs in babies under six months
- Irritability following a cold or respiratory infection
Diagnosis and Treatment Options for Baby Ear Infections
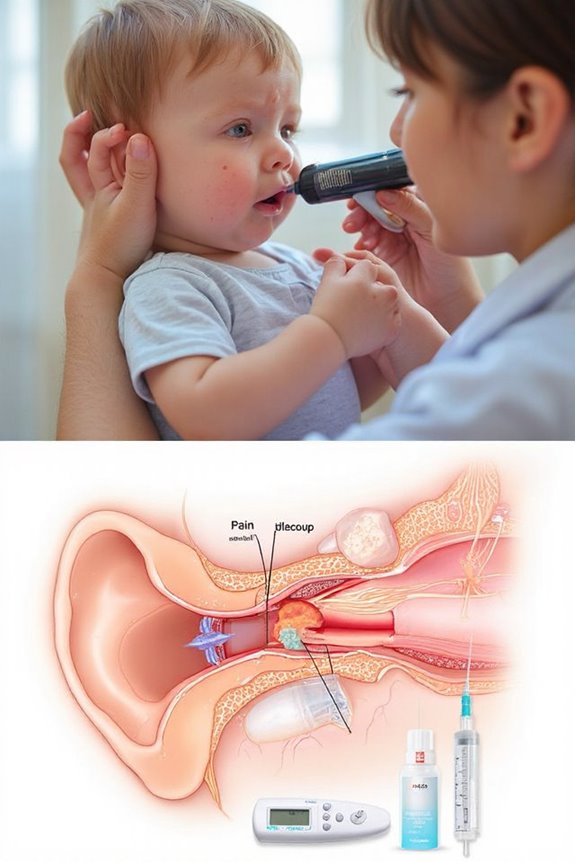
Once your pediatrician suspects an ear infection in your baby, they’ll need to confirm the diagnosis before determining the appropriate treatment. The doctor will typically use an otoscope to visually examine your child’s eardrum for redness, swelling, or fluid.
Diagnostic Methods
- Visual inspection with a lighted otoscope
- Pneumatic otoscope to check eardrum mobility
- Tympanometry to measure ear pressure and detect fluid
Treatment Options
- Watchful waiting for 48-72 hours in mild cases (especially in children over 2)
- Antibiotics for moderate/severe cases or babies under 2 years
- Pain relievers like acetaminophen or ibuprofen
- Follow-up examination to confirm resolution
For recurrent infections, your doctor might refer you to an ENT specialist who may recommend tympanostomy tubes.
Preventing Ear Infections in Your Little One

While treatment is important when your baby has an ear infection, prevention can help you avoid those sleepless nights and doctor visits altogether. I recommend focusing on these key strategies:
- Vaccination strategies: Keep up with pneumococcal and flu vaccines, which greatly reduce ear infection risk.
- Hygiene practices: Wash hands frequently with soap and water, especially before handling your baby.
- Breastfeeding benefits: If possible, breastfeed exclusively for six months. The antibodies in breast milk strengthen your baby’s immune system against infections.
- Environmental considerations: Keep your home smoke-free and limit your baby’s exposure to sick individuals.
- Additional measures: Position your baby upright during feedings, limit pacifier use to bedtime only, and attend regular check-ups for early detection of potential issues.
These simple prevention strategies can dramatically reduce your little one’s risk of developing painful ear infections.
When to Call the Doctor: Red Flags for Parents
As parents, knowing exactly when to seek medical attention for your baby’s ear problems can be challenging. I’ve compiled key emergency signs that warrant immediate medical care:
- High fever (above 102.2°F or 39°C), especially in infants under 3 months
- Severe pain, indicated by inconsolable crying or ear-tugging
- Bloody or pus-like discharge from the ear
- Balance problems or unusual clumsiness
- Apparent hearing difficulty or unresponsiveness to sounds
Parent concerns should never be dismissed. Trust your instincts if your baby’s symptoms persist longer than 24-48 hours or worsen despite home care. Additionally, contact your doctor if your child experiences:
- Multiple ear infections within a short timeframe
- Symptoms that don’t improve after antibiotic treatment
- Unusual drowsiness or lethargy alongside ear discomfort
Frequently Asked Questions
Can Ear Infections Cause Permanent Hearing Loss in Babies?
Ever worry about your baby’s hearing? While rare, untreated ear infections can cause permanent damage. I’ve seen most infants experience complete hearing recovery when infections are promptly addressed by medical professionals.
Are Some Babies Genetically Predisposed to Getting Ear Infections?
Yes, I’ve found that genetic factors play a significant role in ear infection susceptibility. Some babies inherit variations affecting their immune response, with studies showing 40-70% of recurrent infections have a hereditary component.
How Long Does Immunity Last After an Ear Infection?
Particularly puzzling point: I can’t pinpoint a precise immunity duration after ear infections. Your child’s protection varies widely, and ear infection recurrence often depends on their unique immune response rather than a fixed immunity timeframe.
Can Teething Trigger or Worsen Ear Infections?
While teething symptoms don’t directly cause ear infections, they can mimic ear pain. The immune response during teething may be lowered, potentially making your baby more susceptible to infections, including ear infections.
Do Pacifiers Increase the Risk of Ear Infections?
Yes, I’ve found that pacifier usage can triple the risk of ear infections, especially with continuous use. I recommend limiting use, ensuring proper oral hygiene, and considering weaning after 6 months to reduce this risk.





